Guía de práctica clínica para el diagnóstico y tratamiento de la criptococosis en personas adultas que viven con el VIH
Contenido principal del artículo
Resumen
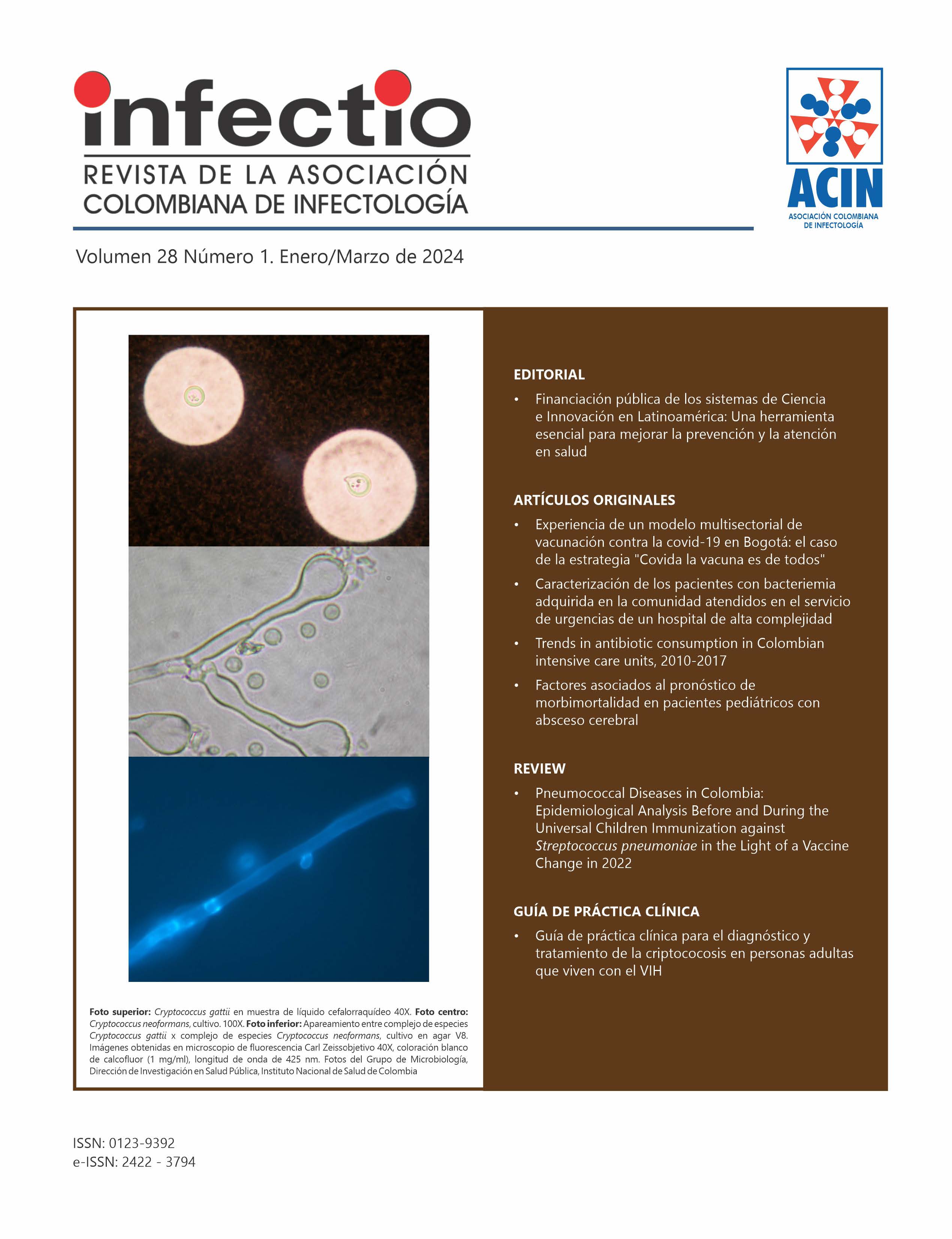
La criptococosis es la infección fúngica ocasionada por el complejo de especies Cryptococcus neoformans y Cryptococcus gattii, desarrollada con mayor frecuencia en personas con compromiso del sistema inmune. En las personas que viven con el virus de la inmunodeficiencia humana (VIH), la criptococosis es una infección oportunista de gran importancia, con consecuencias devastadoras para los pacientes, la sociedad y el sistema de salud, debido al incremento en morbilidad, mortalidad y costos que genera. La presente guía contiene recomendaciones para el diagnóstico y tratamiento de la criptococosis en personas adultas que viven con el VIH, basadas en la evidencia, realizadas mediante el proceso de adaptación de guías de práctica clínica internacionales para el contexto colombiano.
Detalles del artículo
Citas
Levitz SM. The ecology of Cryptococcus neoformans and the epidemiology of cryptococcosis. Rev Infect Dis. 1991;13(6):1163-9. https://doi.org/10.1093/clinids/13.6.1163
Kwon-Chung KJ, Bennett JE, Wickes BL, Meyer W, Cuomo CA, Wollenburg KR, et al. The Case for Adopting the "Species Complex" Nomenclature for the Etiologic Agents of Cryptococcosis. mSphere. 2017;2(1). https://doi.org/10.1128/mSphere.00357-16
May RC, Stone NR, Wiesner DL, Bicanic T, Nielsen K. Cryptococcus: from environmental saprophyte to global pathogen. Nat Rev Microbiol. 2016;14(2):106-17. https://doi.org/10.1038/nrmicro.2015.6
Elsegeiny W, Marr KA, Williamson PR. Immunology of Cryptococcal Infections: Developing a Rational Approach to Patient Therapy. Front Immunol. 2018;9:651. https://doi.org/10.3389/fimmu.2018.00651
Miyazato A. [Mechanism of Cryptococcus Meningoencephalitis]. Med Mycol J. 2016;57(1):J27-32. https://doi.org/10.3314/mmj.57.J27
Esher SK, Zaragoza O, Alspaugh JA. Cryptococcal pathogenic mechanisms: a dangerous trip from the environment to the brain. Mem Inst Oswaldo Cruz. 2018;113(7):e180057. https://doi.org/10.1590/0074-02760180057
Chen Z, Wang N, Huang Y, Wang M. Clinical characteristics and cerebro-spinal fluid cytokine changes in patients with acquired immunodeficiency syndrome and central nervous system infection. Exp Ther Med. 2019;18(1):523-30. https://doi.org/10.3892/etm.2019.7587
Rajasingham R, Smith RM, Park BJ, Jarvis JN, Govender NP, Chiller TM, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis. 2017;17(8):873-81. https://doi.org/10.1016/S1473-3099(17)30243-8
Pasquier E, Kunda J, De Beaudrap P, Loyse A, Temfack E, Molloy SF, et al. Long-term Mortality and Disability in Cryptococcal Meningitis: A Systematic Literature Review. Clin Infect Dis. 2018;66(7):1122-32. https://doi.org/10.1093/cid/cix870
Cuenta de Alto de Costo (CAC), Fondo Colombiano de Enfermedades de Alto Costo, Cuenta de Alto Costo (CAC). Situación del VIH en Colombia, 2022; Bogotá, D.C. 2023.
Escandon P, Lizarazo J, Agudelo CI, Castaneda E. Cryptococcosis in Colombia: Compilation and Analysis of Data from Laboratory-Based Surveillance. J Fungi (Basel). 2018;4(1). https://doi.org/10.3390/jof4010032
Bermas A, Geddes-McAlister J. Combatting the evolution of antifungal resistance in Cryptococcus neoformans. Mol Microbiol. 2020;114(5):721- 34. https://doi.org/10.1111/mmi.14565
WHO fungal priority pathogens list to guide research, development and public health action. Geneva: World Health Organization; 2022. Licence: CC BY-NC-SA 3.0 IGO.
Colombia. Ministerio de Salud y Protección Social. Guía Metodológica, Adopción Adaptación de Guías de Práctica Clínica Basadas en Evidencia. Guía metodológica en Internet. Edición 1ª. Bogotá DC. 2017, Disponible en gpc.minsalud.gov.co.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839-42. https://doi.org/10.1503/cmaj.090449
Schunemann HJ, Wiercioch W, Brozek J, Etxeandia-Ikobaltzeta I, Mustafa RA, Manja V, et al. GRADE Evidence to Decision (EtD) frameworks for adoption, adaptation, and de novo development of trustworthy recommendations: GRADE-ADOLOPMENT. J Clin Epidemiol. 2017;81:101- 10. https://doi.org/10.1016/j.jclinepi.2016.09.009
Schunemann HJ, Mustafa R, Brozek J, Santesso N, Alonso-Coello P, Guyatt G, et al. GRADE Guidelines: 16. GRADE evidence to decision frameworks for tests in clinical practice and public health. J Clin Epidemiol. 2016;76:89- 98. https://doi.org/10.1016/j.jclinepi.2016.01.032
Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401-6. https://doi.org/10.1016/j.jclinepi.2010.07.015 https://doi.org/10.1016/j.jclinepi.2010.07.015
Gutierrez GC, Pulido Álvarez AC, de la Hoz AM, Alviar KM, Muñoz Velandia ÓM, Guerrero Carvajar R, et al. Guía Metodológica para la elaboración de Guías de Práctica Clínica con Evaluación Económica en el Sistema General de Seguridad Social en Salud Colombiano Bogotá DC: Fundación Santa Fe de Bogotá - Centro de Estudios e Investigación en Salud; 2014.
Andrews J, Guyatt G, Oxman AD, Alderson P, Dahm P, Falck-Ytter Y, et al. GRADE guidelines: 14. Going from evidence to recommendations: the significance and presentation of recommendations. J Clin Epidemiol. 2013;66(7):719-25. https://doi.org/10.1016/j.jclinepi.2012.03.013
Haas AD, Radin E, Birhanu S, Low AJ, Saito S, Sachathep K, et al. Prevalence of and factors associated with late diagnosis of HIV in Malawi, Zambia, and Zimbabwe: Results from population-based nationally representative surveys. PLOS Glob Public Health. 2022;2(2):e0000080. https://doi.org/10.1371/journal.pgph.0000080
Reus S, Portilla, J., Gimeno, A., Sánchez-Payá, J., García-Henarejos, J. A., Martínez-Madrid, O. Predictors of progression and death in patients with advanced HIV infection in the era of highly active antiretroviral therapy. Enferm Infecc Microbiol Clin 2004;22(3):142-9. https://doi.org/10.1157/13058022
Meya DB, Kiragga AN, Nalintya E, Morawski BM, Rajasingham R, Park BJ, et al. Reflexive Laboratory-Based Cryptococcal Antigen Screening and Preemptive Fluconazole Therapy for Cryptococcal Antigenemia in HIV-Infected Individuals With CD4 <100 Cells/microL: A Stepped-Wedge, Cluster-Randomized Trial. J Acquir Immune Defic Syndr. 2019;80(2):182-9. https://doi.org/10.1097/QAI.0000000000001894
Powderly WG, Cloud GA, Dismukes WE, Saag MS. Measurement of cryptococcal antigen in serum and cerebrospinal fluid: value in the management of AIDS-associated cryptococcal meningitis. Clin Infect Dis. 1994;18(5):789-92. https://doi.org/10.1093/clinids/18.5.789
Williams DA, Kiiza T, Kwizera R, Kiggundu R, Velamakanni S, Meya DB, et al. Evaluation of fingerstick cryptococcal antigen lateral flow assay in HIV-infected persons: a diagnostic accuracy study. Clin Infect Dis. 2015;61(3):464-7. https://doi.org/10.1093/cid/civ263
Govender NP, Meintjes G, Mangena P, Nel J, Potgieter S, Reddy D, et al. Southern African HIV Clinicians Society guideline for the prevention, diagnosis and management of cryptococcal disease among HIV-infected persons: 2019 update. South Afr J HIV Med. 2019;20(1):1030. https://doi.org/10.4102/sajhivmed.v20i1.1030
Chang CC, Hall V, Cooper C, Grigoriadis G, Beardsley J, Sorrell TC, et al. Consensus guidelines for the diagnosis and management of cryptococcosis and rare yeast infections in the haematology/oncology setting, 2021. Intern Med J. 2021;51 Suppl 7:118-42. https://doi.org/10.1111/imj.15590
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010;50(3):291-322. https://doi.org/10.1086/649858
Guidelines for diagnosing, preventing and managing cryptococcal disease among adults, adolescents and children living with HIV. Geneva: World Health Organization; 2022. Licence: CC BY-NC-SA 3.0 IGO.
Ford N, Shubber Z, Jarvis JN, Chiller T, Greene G, Migone C, et al. CD4 Cell Count Threshold for Cryptococcal Antigen Screening of HIV-Infected Individuals: A Systematic Review and Meta-analysis. Clin Infect Dis. 2018;66(suppl_2):S152-S9. https://doi.org/10.1093/cid/cix1143
Awotiwon AA, Johnson S, Rutherford GW, Meintjes G, Eshun-Wilson I. Primary antifungal prophylaxis for cryptococcal disease in HIV-positive people. Cochrane Database Syst Rev. 2018;8(8):CD004773. https://doi.org/10.1002/14651858.CD004773.pub3
Perfect JR, Bicanic T. Cryptococcosis diagnosis and treatment: What do we know now. Fungal Genet Biol. 2015;78:49-54. https://doi.org/10.1016/j.fgb.2014.10.003
Rajasingham R, Wake RM, Beyene T, Katende A, Letang E, Boulware DR. Cryptococcal Meningitis Diagnostics and Screening in the Era of Point-of- Care Laboratory Testing. J Clin Microbiol. 2019;57(1). https://doi.org/10.1128/JCM.01238-18
Abassi M, Boulware DR, Rhein J. Cryptococcal Meningitis: Diagnosis and Management Update. Curr Trop Med Rep. 2015;2(2):90-9. https://doi.org/10.1007/s40475-015-0046-y
Antinori S, Galimberti L, Magni C, Casella A, Vago L, Mainini F, et al. Cryptococcus neoformans infection in a cohort of Italian AIDS patients: natural history, early prognostic parameters, and autopsy findings. Eur J Clin Microbiol Infect Dis. 2001;20(10):711-7. https://doi.org/10.1007/s100960100616
Batungwanayo J, Taelman H, Bogaerts J, Allen S, Lucas S, Kagame A, et al. Pulmonary cryptococcosis associated with HIV-1 infection in Rwanda: a retrospective study of 37 cases. AIDS. 1994;8(9):1271-6. https://doi.org/10.1097/00002030-199409000-00008
Bogaerts J, Rouvroy D, Taelman H, Kagame A, Aziz MA, Swinne D, et al. AIDS-associated cryptococcal meningitis in Rwanda (1983-1992): epidemiologic and diagnostic features. J Infect. 1999;39(1):32-7. https://doi.org/10.1016/S0163-4453(99)90099-3
Calvo B, Fischman O, Castelo Filho A, Reis Filho J, Del Bianco R, Barbosa RM, et al. [Detection of capsular polysaccharide antigen of Cryptococcus neoformans in patients with AIDS and neurocryptococcosis in Sao Paulo, Brazil]. Rev Inst Med Trop Sao Paulo. 1991;33(6):485-90.
https://doi.org/10.1590/S0036-46651991000600009
Chen S, Sorrell T, Nimmo G, Speed B, Currie B, Ellis D, et al. Epidemiology and host- and variety-dependent characteristics of infection due to Cryptococcus neoformans in Australia and New Zealand. Australasian Cryptococcal Study Group. Clin Infect Dis. 2000;31(2):499-508. https://doi.org/10.1086/313992
Chuck SL, Sande MA. Infections with Cryptococcus neoformans in the acquired immunodeficiency syndrome. N Engl J Med. 1989;321(12):794-9. https://doi.org/10.1056/NEJM198909213211205
Desmet P, Kayembe KD, De Vroey C. The value of cryptococcal serum antigen screening among HIV-positive/AIDS patients in Kinshasa, Zaire. AIDS. 1989;3(2):77-8. https://doi.org/10.1097/00002030-198902000-00004
Likasitwattanakul S, Poneprasert B, Sirisanthana V. Cryptococcosis in HIV infected children. Southeast Asian J Trop Med Public Health. 2004;34:935- 9.
Lin TY, Yeh KM, Lin JC, Wang NC, Peng MY, Chang FY. Cryptococcal disease in patients with or without human immunodeficiency virus: clinical presentation and monitoring of serum cryptococcal antigen titers. J Microbiol Immunol Infect. 2009;42(3):220-6.
McCarthy KM, Morgan J, Wannemuehler KA, Mirza SA, Gould SM, Mhlongo N, et al. Population-based surveillance for cryptococcosis in an antiretroviral-naive South African province with a high HIV seroprevalence. AIDS. 2006;20(17):2199-206. https://doi.org/10.1097/QAD.0b013e3280106d6a
Rozenbaum R, Goncalves AJ. Clinical epidemiological study of 171 cases of cryptococcosis. Clin Infect Dis. 1994;18(3):369-80. https://doi.org/10.1093/clinids/18.3.369
Saha DC, Xess I, Biswas A, Bhowmik DM, Padma MV. Detection of Cryptococcus by conventional, serological and molecular methods. J Med Microbiol. 2009;58(Pt 8):1098-105. https://doi.org/10.1099/jmm.0.007328-0
Sekhon AS, Garg AK, Kaufman L, Kobayashi GS, Hamir Z, Jalbert M, et al. Evaluation of a commercial enzyme immunoassay for the detection of cryptococcal antigen. Mycoses. 1993;36(1-2):31-4. https://doi.org/10.1111/j.1439-0507.1993.tb00684.x
Swinne D, Bogaerts J, Van de Perre P, Batungwanayo J, Taelman H. Evaluation of the cryptococcal antigen test as a diagnostic tool of AIDS-associated cryptococcosis in Rwanda. Ann Soc Belg Med Trop. 1992;72(4):283-8.
Tanner DC, Weinstein MP, Fedorciw B, Joho KL, Thorpe JJ, Reller L. Comparison of commercial kits for detection of cryptococcal antigen. J Clin Microbiol. 1994;32(7):1680-4. https://doi.org/10.1128/jcm.32.7.1680-1684.1994
Wadhwa A, Kaur R, Bhalla P. Profile of central nervous system disease in HIV/AIDS patients with special reference to cryptococcal infections. Neurologist. 2008;14(4):247-51. https://doi.org/10.1097/NRL.0b013e3181678a7a
Rutherford G, Horvath H, Anglemyer A. Diagnosis of and screening for cryptococcal infection in people with HIV: Systematic review and GRADE evidence profiles2015.
Jarvis JN, Meintjes G, Williams A, Brown Y, Crede T, Harrison TS. Adult meningitis in a setting of high HIV and TB prevalence: findings from 4961 suspected cases. BMC Infect Dis. 2010;10:67. https://doi.org/10.1186/1471-2334-10-67
Sathyanarayanan V, Razak A, Chakraborty J. Clinical profile of disseminated cryptococcal infection - a case series. Asian Pacific Trop Med. 2010;3:818- 20.
https://doi.org/10.1016/S1995-7645(10)60197-6
Nelson MR, Bower M, Smith D, Reed C, Shanson D, Gazzard B. The value of serum cryptococcal antigen in the diagnosis of cryptococcal infection in patients infected with the human immunodeficiency virus. J Infect. 1990;21(2):175-81. https://doi.org/10.1016/0163-4453(90)91727-U
French N, Gray K, Watera C, Nakiyingi J, Lugada E, Moore M, et al. Cryptococcal infection in a cohort of HIV-1-infected Ugandan adults. AIDS. 2002;16(7):1031-8. https://doi.org/10.1097/00002030-200205030-00009
Jarvis JN, Percival A, Bauman S, Pelfrey J, Meintjes G, Williams GN, et al. Evaluation of a novel point-of-care cryptococcal antigen test on serum, plasma, and urine from patients with HIV-associated cryptococcal meningitis. Clin Infect Dis. 2011;53(10):1019-23. https://doi.org/10.1093/cid/cir613
Lindsley MD, Mekha N, Baggett HC, Surinthong Y, Autthateinchai R, Sawatwong P, et al. Evaluation of a newly developed lateral flow immunoassay for the diagnosis of cryptococcosis. Clin Infect Dis. 2011;53(4):321-5.
https://doi.org/10.1093/cid/cir379
Helou S, Robles AM, Arechavala AI, Bianchi MH, Negroni R. [Respiratory cryptococcosis in HIV positive patients.]. Rev Iberoam Micol. 1999;16(3):126-9.
Taelman H, Bogaerts J, Batungwanayo J, Van de Perre P, Lucas S, Allen S. Failure of the cryptococcal serum antigen test to detect primary pulmonary cryptococcosis in patients infected with human immunodeficiency virus. Clin Infect Dis. 1994;18(1):119-20. https://doi.org/10.1093/clinids/18.1.119
Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267-84. https://doi.org/10.1086/425368
van de Beek D, Cabellos C, Dzupova O, Esposito S, Klein M, Kloek AT, et al. ESCMID guideline: diagnosis and treatment of acute bacterial meningitis. Clin Microbiol Infect. 2016;22 Suppl 3:S37-62. https://doi.org/10.1016/j.cmi.2016.01.007
McGill F, Heyderman RS, Michael BD, Defres S, Beeching NJ, Borrow R, et al. The UK joint specialist societies guideline on the diagnosis and management of acute meningitis and meningococcal sepsis in immunocompetent adults. J Infect. 2016;72(4):405-38.
https://doi.org/10.1016/j.jinf.2016.01.007
Glimaker M, Johansson B, Bell M, Ericsson M, Blackberg J, Brink M, et al. Early lumbar puncture in adult bacterial meningitis--rationale for revised guidelines. Scand J Infect Dis. 2013;45(9):657-63. https://doi.org/10.3109/00365548.2013.799289
Park N, Nigo M, Hasbun R. Comparison of Four International Guidelines on the Utility of Cranial Imaging Before Lumbar Puncture in Adults with Bacterial Meningitis. Clin Neuroradiol. 2022;32(3):857-62. https://doi.org/10.1007/s00062-022-01143-4
Tenforde MW, Shapiro AE, Rouse B, Jarvis JN, Li T, Eshun-Wilson I, et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018;7(7):CD005647. https://doi.org/10.1002/14651858
Bicanic T, Bottomley C, Loyse A, Brouwer AE, Muzoora C, Taseera K, et al. Toxicity of Amphotericin B Deoxycholate-Based Induction Therapy in Patients with HIV-Associated Cryptococcal Meningitis. Antimicrob Agents Chemother. 2015;59(12):7224-31. https://doi.org/10.1128/AAC.01698-15
Vermes A, Guchelaar HJ, Dankert J. Flucytosine: a review of its pharmacology, clinical indications, pharmacokinetics, toxicity and drug interactions. J Antimicrob Chemother. 2000;46(2):171-9. https://doi.org/10.1093/jac/46.2.171
Bicanic T, Harrison T, Niepieklo A, Dyakopu N, Meintjes G. Symptomatic relapse of HIV-associated cryptococcal meningitis after initial fluconazole monotherapy: the role of fluconazole resistance and immune reconstitution. Clin Infect Dis. 2006;43(8):1069-73. https://doi.org/10.1086/507895
Molloy SF, Kanyama C, Heyderman RS, Loyse A, Kouanfack C, Chanda D, et al. Antifungal Combinations for Treatment of Cryptococcal Meningitis in Africa. N Engl J Med. 2018;378(11):1004-17. https://doi.org/10.1056/NEJMoa1710922
Day JN, Chau TTH, Wolbers M, Mai PP, Dung NT, Mai NH, et al. Combination antifungal therapy for cryptococcal meningitis. N Engl J Med. 2013;368(14):1291-302. https://doi.org/10.1056/NEJMoa1110404
Brouwer AE, Rajanuwong A, Chierakul W, Griffin GE, Larsen RA, White NJ, et al. Combination antifungal therapies for HIV-associated cryptococcal meningitis: a randomised trial. Lancet. 2004;363(9423):1764-7. https://doi.org/10.1016/S0140-6736(04)16301-0
Pappas PG, Chetchotisakd P, Larsen RA, Manosuthi W, Morris MI, Anekthananon T, et al. A phase II randomized trial of amphotericin B alone or combined with fluconazole in the treatment of HIV-associated cryptococcal meningitis. Clin Infect Dis. 2009;48(12):1775-83. https://doi.org/10.1086/599112
Shapiro AE, Tenforde MW, Chiller TM, Ford N, Rajasingham R. An updated systematic review of HIV-associated cryptococcal meningitis treatment strategies. HIV Med. 2023;24(4):507-12. https://doi.org/10.1111/hiv.13412
Jarvis JN, Lawrence DS, Meya DB, Kagimu E, Kasibante J, Mpoza E, et al. Single-Dose Liposomal Amphotericin B Treatment for Cryptococcal Meningitis. N Engl J Med. 2022;386(12):1109-20. https://doi.org/10.1056/NEJMoa2111904
Lawrence DS, Ssali A, Moshashane N, Nabaggala G, Maphane L, Harrison TS, et al. Decision making in a clinical trial for a life-threatening illness: Therapeutic expectation, not misconception. Soc Sci Med. 2022;305:115082. https://doi.org/10.1016/j.socscimed.2022.115082
Martin MV. The use of fluconazole and itraconazole in the treatment of Candida albicans infections: a review. J Antimicrob Chemother. 1999;44(4):429-37. https://doi.org/10.1093/jac/44.4.429
Nocua-Baez LC, Uribe-Jerez P, Tarazona-Guaranga L, Robles R, Cortes JA. [Azoles of then and now: a review]. Rev Chilena Infectol. 2020;37(3):219- 30. https://doi.org/10.4067/s0716-10182020000300219
Albengres E, Le Louet H, Tillement JP. Systemic antifungal agents. Drug interactions of clinical significance. Drug Saf. 1998;18(2):83-97. https://doi.org/10.2165/00002018-199818020-00001
Bates DW, Yu DT. Clinical impact of drug-drug interactions with systemic azole antifungals. Drugs Today (Barc). 2003;39(10):801-13. https://doi.org/10.1358/dot.2003.39.10.799473
van der Horst CM, Saag MS, Cloud GA, Hamill RJ, Graybill JR, Sobel JD, et al. Treatment of cryptococcal meningitis associated with the acquired immunodeficiency syndrome. National Institute of Allergy and Infectious Diseases Mycoses Study Group and AIDS Clinical Trials Group. N Engl J Med. 1997;337(1):15-21. https://doi.org/10.1056/NEJM199707033370103
Mootsikapun P, Chetchotisakd P, Anunnatsiri S, Choksawadphinyo K. The efficacy of fluconazole 600 mg/day versus itraconazole 600 mg/day as consolidation therapy of cryptococcal meningitis in AIDS patients. J Med Assoc Thai. 2003;86(4):293-8.
Ngan NTT, Flower B, Day JN. Treatment of Cryptococcal Meningitis: How Have We Got Here and Where are We Going? Drugs. 2022;82(12):1237-49.
https://doi.org/10.1007/s40265-022-01757-5
Bozzette SA, Larsen RA, Chiu J, Leal MA, Jacobsen J, Rothman P, et al. A placebo-controlled trial of maintenance therapy with fluconazole after treatment of cryptococcal meningitis in the acquired immunodeficiency syndrome. California Collaborative Treatment Group. N Engl J Med. 1991;324(9):580-4. https://doi.org/10.1056/NEJM199102283240902
Saag MS, Cloud GA, Graybill JR, Sobel JD, Tuazon CU, Johnson PC, et al. A comparison of itraconazole versus fluconazole as maintenance therapy for AIDS-associated cryptococcal meningitis. National Institute of Allergy and Infectious Diseases Mycoses Study Group. Clin Infect Dis. 1999;28(2):291-6. https://doi.org/10.1086/515110
Powderly WG, Saag MS, Cloud GA, Robinson P, Meyer RD, Jacobson JM, et al. A controlled trial of fluconazole or amphotericin B to prevent relapse of cryptococcal meningitis in patients with the acquired immunodeficiency syndrome. The NIAID AIDS Clinical Trials Group and Mycoses Study Group. N Engl J Med. 1992;326(12):793-8.
https://doi.org/10.1056/NEJM199203193261203
Quagliarello V, Scheld WM. Bacterial meningitis: pathogenesis, pathophysiology, and progress. N Engl J Med. 1992;327(12):864-72.
https://doi.org/10.1056/NEJM199209173271208
Tauber MG, Khayam-Bashi H, Sande MA. Effects of ampicillin and corticosteroids on brain water content, cerebrospinal fluid pressure, and cerebrospinal fluid lactate levels in experimental pneumococcal meningitis. J Infect Dis. 1985;151(3):528-34. https://doi.org/10.1093/infdis/151.3.528
Girgis NI, Farid Z, Mikhail IA, Farrag I, Sultan Y, Kilpatrick ME. Dexamethasone treatment for bacterial meningitis in children and adults. Pediatr Infect Dis J. 1989;8(12):848-51. https://doi.org/10.1097/00006454-198912000-00004
McIntyre PB, Berkey CS, King SM, Schaad UB, Kilpi T, Kanra GY, et al. Dexamethasone as adjunctive therapy in bacterial meningitis. A meta-analysis of randomized clinical trials since 1988. JAMA. 1997;278(11):925- 31. https://doi.org/10.1001/jama.278.11.925
Scarborough M, Gordon SB, Whitty CJ, French N, Njalale Y, Chitani A, et al. Corticosteroids for bacterial meningitis in adults in sub-Saharan Africa. N Engl J Med. 2007;357(24):2441-50. https://doi.org/10.1056/NEJMoa065711
Beardsley J, Wolbers M, Kibengo FM, Ggayi AB, Kamali A, Cuc NT, et al. Adjunctive Dexamethasone in HIV-Associated Cryptococcal Meningitis. N Engl J Med. 2016;374(6):542-54. https://doi.org/10.1056/NEJMoa1509024
The White House. 2021. National HIV/AIDS Strategy for the United States 2022-2025. Washington, DC.
Haddow LJ, Colebunders R, Meintjes G, Lawn SD, Elliott JH, Manabe YC, et al. Cryptococcal immune reconstitution inflammatory syndrome in HIV-1- infected individuals: proposed clinical case definitions. Lancet Infect Dis. 2010;10(11):791-802. https://doi.org/10.1016/S1473-3099(10)70170-5
Group ISS, Lundgren JD, Babiker AG, Gordin F, Emery S, Grund B, et al. Initiation of Antiretroviral Therapy in Early Asymptomatic HIV Infection. N Engl J Med. 2015;373(9):795-807. https://doi.org/10.1056/NEJMoa1506816
Eshun-Wilson I, Okwen MP, Richardson M, Bicanic T. Early versus delayed antiretroviral treatment in HIV-positive people with cryptococcal meningitis. Cochrane Database Syst Rev. 2018;7(7):CD009012. https://doi.org/10.1002/14651858.CD009012.pub3
Bisson GP, Molefi M, Bellamy S, Thakur R, Steenhoff A, Tamuhla N, et al. Early versus delayed antiretroviral therapy and cerebrospinal fluid fungal clearance in adults with HIV and cryptococcal meningitis. Clin Infect Dis. 2013;56(8):1165-73. https://doi.org/10.1093/cid/cit019
Boulware DR, Meya DB, Muzoora C, Rolfes MA, Huppler Hullsiek K, Musubire A, et al. Timing of antiretroviral therapy after diagnosis of cryptococcal meningitis. N Engl J Med. 2014;370(26):2487-98. https://doi.org/10.1056/NEJMoa1312884
Makadzange AT, Ndhlovu CE, Takarinda K, Reid M, Kurangwa M, Gona P, et al. Early versus delayed initiation of antiretroviral therapy for concurrent HIV infection and cryptococcal meningitis in sub-saharan Africa. Clin Infect Dis. 2010;50(11):1532-8. https://doi.org/10.1086/652652
Zolopa A, Andersen J, Powderly W, Sanchez A, Sanne I, Suckow C, et al. Early antiretroviral therapy reduces AIDS progression/death in individuals with acute opportunistic infections: a multicenter randomized strategy trial. PLoS One. 2009;4(5):e5575. https://doi.org/10.1371/journal.pone.0005575